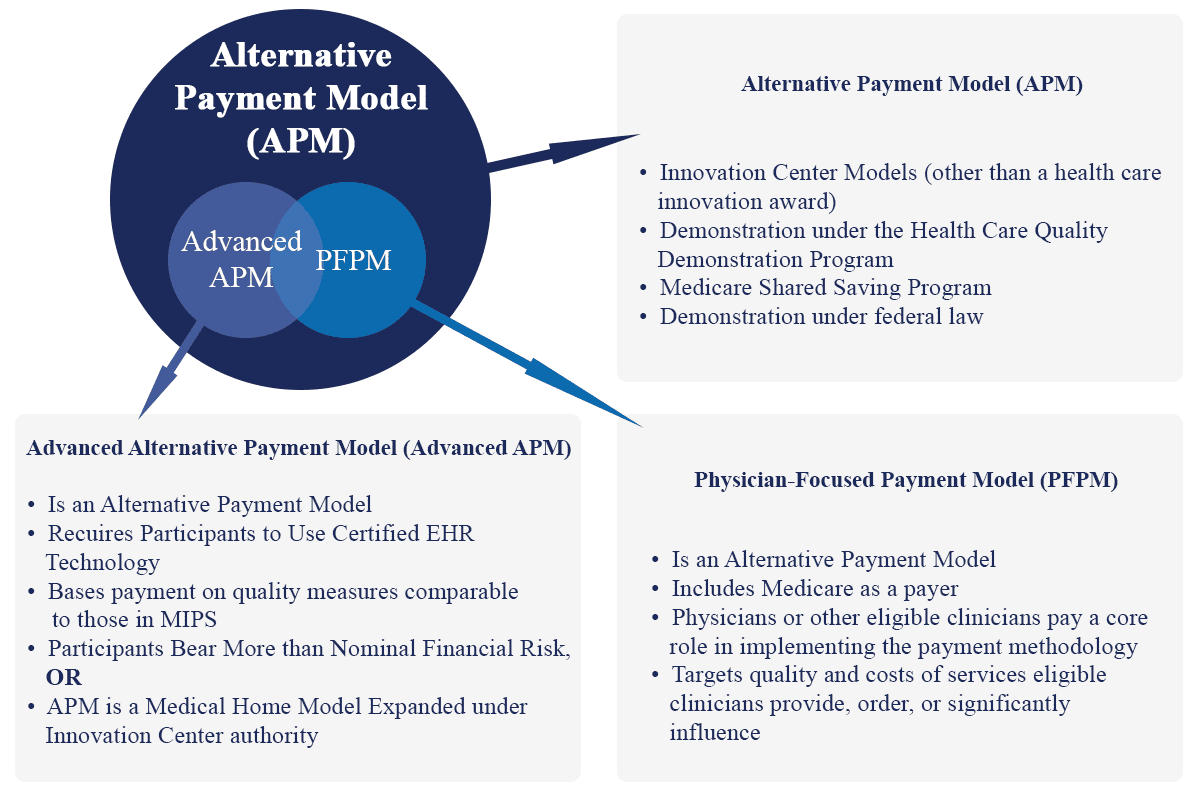
According, to CMS definition an Alternative Payment Model (APM) is a new payment approach or model, developed in collaboration with the provider community, that grants additional incentives to clinicians to provide high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population.
Advanced APM
Advanced APMs are a subset of APMs and allow practices to earn more incentives for taking on risk related to patients’ outcomes. As an Advanced APM participant providers may earn a 5% Medicare incentive payment during 2019 through 2024 and will be exempt from MIPS reporting requirements and payment adjustments if the provider has a sufficient level of participation in an Advanced APM. However, bear in mind that earning an incentive payment in one year does not guarantee to receive the incentive payment in years to come.
Advanced APMs (according to CMS) must meet the following requirements:
- Be CMS Innovation Center models, Shared Savings Program tracks, or certain federal demonstration programs
- Require participants to use certified EHR technology
- Base payments for services on quality measures comparable to those in MIPS
- Be a Medical Home Model expanded under Innovation Center authority or require participants to bear more than nominal financial risk for losses. The final rule with comment period defined the risk requirement for an Advanced APM to be in terms of either total Medicare expenditures or participating organizations’ Medicare revenue (which may vary significantly).