Medicare pays separately under the Medicare Physician Fee Schedule for non-face-to-face care coordination services furnished to Medicare beneficiaries with multiple chronic conditions. The reimbursement per qualifying patient per month is $79.26.
Why the Need for the General Care Management Program?
What is General Care Management Reimbursement (GCM) for CPT Code G0511?
- Multiple (two or more) chronic conditions expected to last at least 12 months, or until the death of the patient.
- Chronic conditions place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline.
- Comprehensive care management plan established, implemented, revised, or monitored.
New conditions are being added as CMS has elaborated on the definition of a chronic condition. Examples of chronic conditions include:
Alzheimer’s disease and related dementia
Chronic Kidney Disease
Cancer (almost all cancers)
Glaucoma
Anemia
Asthma
Chronic Obstructive Pulmonary Disease
Diabetes
Hypertension
Osteoporosis
Chronic Pain & Fatigue
Atrial Fibrillation
Obesity Stroke
Cataract
Arthritis (osteoarthritis and rheumatoid)
Autism Spectrum Disorders
Depression
Heart Failure
Ischemic Heart Disease
Migraine/ Chronic Headache
Fibromyalgia
Physicians and the following non-physician practitioners may bill the new GCM service:
Certified Nurse Midwives
Clinical Nurse Specialists
Nurse Practitioners
Physician Assistants
Only one practitioner may be paid for the GCM service for a given calendar month.
Note: Eligible practitioners must act within their State licensure, scope of practice and Medicare statutory benefit. The GCM service may be billed most frequently by primary care physicians, although specialty physicians who meet all of the billing requirements may bill the service. The GCM service is not within the scope of practice of limited license physicians and practitioners such as clinical physiologists, podiatrists, or dentists, therefore these practitioners cannot furnish or bill the service. However, CMS expects referral or consultation with such physicians and practitioners by the billing practitioner to coordinate and manage care.
CMS provided an exception under Medicare’s “incident to” rules that permits GCM clinical staff to provide the GCM service incident to the services of the billing physician (or other appropriate practitioner) under the general supervision (rather than direct supervision) of a physician (or other appropriate practitioner).
We provide all the tools and resources needed to Participate in the GCM Program and allow you to begin receiving the Financial Benefits quickly while improving the health of your chronically ill Medicare patients. We do all the work, which gives you access to this Incentive Money without placing the burden on your practice or your staff!

What are the Benefits of General Care Management?
Providers
Make up to $300,000 a year gross annual revenue through care management reimbursement
We schedule all the GCM patients preventative and health maintenance appointments increasing in-office encounter revenue 20%- 30% on average
Improve your quality measures for other incentive programs
Stay focused on in-office patient care and let our staff provide the remote patient monitoring and remote therapeutic monitoring services your chronically ill Medicare patients need to improve their health.
Free up time to either enjoy time outside of the office or potentially see more patients
Satisfied patients are more likely to adhere to their care plans and continue to be treated by providers that are invested in improving their health. Telehealth services are just one more touch point to aid patients in their chronic care management.
CMS provided an exception under Medicare’s “incident to” rules that permits clinical staff to provide the GCM service incident to the services of the billing physician (or other appropriate practitioner) under the general supervision (rather than direct supervision) of a physician (or other appropriate practitioner).
We provide all the tools and resources needed to Participate in the GCM Program and allow you to begin receiving the Financial Benefits quickly while improving the health of your chronically ill Medicare patients. We do all the work, which gives you access to this Incentive Money without placing burden on your practice or your staff!
CMS provided an exception under Medicare’s “incident to” rules that permits clinical staff to provide the GCM service incident to the services of the billing physician (or other appropriate practitioner) under the general supervision (rather than direct supervision) of a physician (or other appropriate practitioner).
We provide all the tools and resources needed to Participate in the GCM Program and allow you to begin receiving the Financial Benefits quickly while improving the health of your chronically ill Medicare patients. We do all the work, which gives you access to this Incentive Money without placing burden on your practice or your staff!
Patients
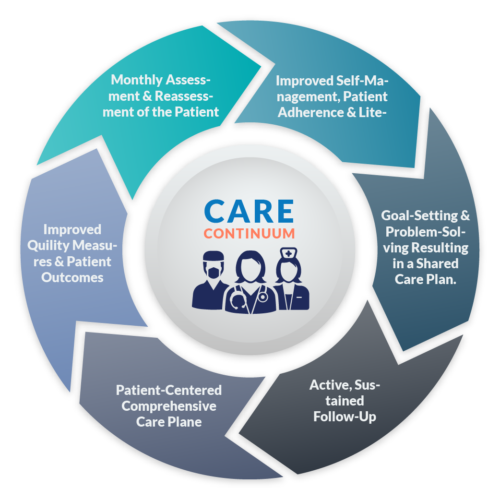
Care Management services provide a continuum of care for patients to improve patient outcomes and reduce total cost of care
Providing 24/7 access to care provides patients with the support needed to better manage their chronic conditions and overall quality of life
Continued care management of the patient improves adherence and patient literacy so they can take an active role and proactive approach to managing their overall health including diet, exercise and nutrition
Care management support addresses gaps in care, provides assistance managing chronic conditions and episodic problems that may otherwise go unaddressed, resulting in poor patient outcomes, costly hospitalizations, procedures or additional chronic disease states
Improved patient adherence and compliance starts with education and literacy. By providing essential patient-centric information patients can understand the need for compliance and be better informed to make the correct decisions in self- management
Patients participating in the GCM program have access to 24/7 care support provided by our RN Clinical Care Team
What are the Challenges to Value-based Care?
Burden Of Time
Managing Internal Resources
Protecting (ePHI)
Cost of Resources
Liability
Compliance
Third-Party software
Documenting Appropriately
Fear of Penalties
Hiring the Right Resources
Additional FAQs Pertaining to GCM
Do you have any sense of what percentage of eligible patients would engage in this type of service? Is there a benchmark for participation in GCM programs?
Even though billing GCM is not exactly the same as CCM, the Center for Primary Care (CPC), featured in the webinar, estimates 75% of eligible patients will consent to participate in CPC’s chronic care management program. Of those, they anticipate approximately 50% will remain compliant and meet the requirements to bill CMS.
CPC provides one reference point for providers interested to forecast program impact. However, patient engagement rates can vary dramatically based upon a host of variables. For this reason, it is critical that providers have a deliberate strategy to educate beneficiaries and secure their consent. To discuss program modeling or for further information related to patient engagement, please contact us directly.
How do you identify all the qualifying Medicare patients?
We use our sophisticated software tool to identify all your qualifying CCM patients, we also have experience working on over 150 EHR, PMS and Patient Portal systems, which makes us intimately familiar with the features and functionality of the technologies you have in place and we have the experience to pull the reports from your systems in order to cross map with our tool to determine all your qualifying GCM patients.
Since patients are required to pay a coinsurance under this program, won’t that dissuade most from participating?
Only one in 10 beneficiaries relies solely on the Medicare program for health care coverage. The rest have some form of supplemental coverage to help with medical expenses, so 70% of your patients may not have to pay out of pocket for the co-insurance.
Is there a list of chronic conditions that qualify under the program?
CMS maintains a Chronic Condition Warehouse (CCW) that includes information on 70+ specified chronic conditions. However, the CCW list is not an exclusive list of chronic conditions; CMS may recognize other conditions for purposes of providing GCM such as Psychiatric and Behavioral conditions that may not be listed CCW.
Do Remote Patient Monitoring and Remote Therapeutic Monitoring Services qualify for GCM Reimbursement?
The time spent for Remote Patient Monitoring and Remote Therapeutic Monitoring can be added to the total time spent for GCM services for the month and once the scope of service for GCM services is met for the month the FQHC/ RHC can bill CPT code G0511. As of 2022, there is no separate CPT billing code for FQHCs or RHCs to be able to bill separately for these services.
How can your practice use Transitional Care Management to help patients find success at home?
As part of the scope of providing General Care Management services for your patients each month if a patient needs transitional care management services they need to be provided prior t billing CPT Code G)511 and documented as part of your GCM note. Transitional Care Management services are very helpful to a patient to help the patient transition to their home and avoid patient readmissions and keep them healthy in their home.
Many of these services can include communicating with other community services utilized by patient; educate patient and/or family/caretaker regarding self-management, independent living, and activities of daily living; assess and support treatment regimen adherence and medication management; identify available community and health resources; and facilitate access to necessary care and services.
Will Medicare Advantage (MA) plans reimburse for GCM? What about commercial payers?
A Medicare Advantage plan is required to offer its enrollees at least traditional Medicare benefits, which now will include GCM. It seems reasonable to assume that an MA plan will pay for GCM just as it now pays for other physician services. Whether commercial payers will pay for GCM remains to be seen, although the fact that CMS is paying for this service makes it more likely.
We are still unsure about how to effectively "sell" the 20% coinsurance to patients who question why they aren't already receiving that level of care coordination.
Our outreach program is unmatched we have dedicated scripts and value statements to help the chronically ill Medicare beneficiary understand the value and benefit to them as a patient who needs support and guidance to assist them in managing their health. After the consent form has been received by our clinical care managers (RNs) carefully track and monitor the patients, guaranteeing the most effective coordination of care with external providers and agencies. We also provide better access to care for the patients and facilitate scheduling and transportation to their in-office appointments.
Are there specific documentation requirements for the 20 minutes of non-face-to-face services?
The GCM regulations do not require a specific type of documentation of the 20 minutes of non-face-to-face services, nor has CMS issues any guidance on this issue. In the event a provider’s records were to be audited, having the start and stop time recorded for each service would provide the best defense to any challenge. However, having the start and stop times for some services but not others would likely lead to additional inquiries from the auditors. For this reason, the better practice is to document (1) the total amount of time spent, (2) the identity of the person providing the service, and (3) a description of the service rendered. Again, CMS has not specifically required this level of documentation; this is instead a best practice to protect an organization in the event of any audit.
We have some of our patients enrolled, billed, and paid. However, patient engagement remains a challenge and we don’t have the resources to manage the remaining patient load for all of our qualifying GCM patients, can you help?
Yes, there is no practice too big or too small, we work with all providers and all patient populations, we understand the true intent and spirit of CMS and we want to bring value to as many providers and patients as possible. We and our Clinical Care Managers are enthusiastic endorsers of the GCM program.
Can the time spent and documented by home health be counted toward the 20 minutes per month?
If this time is part of an otherwise billable home health service, it cannot be applied or counted toward the 20 minute requirement. CMS would characterize this as “double-dipping.”
If you provide more than 20 minutes of non-face-to-face care during the month, can you bill for the extra time in the month that follows?
CMS requires participating providers who bill CPT Code G0511 to deliver at least 20 minutes of non-face- to- face care to Medicare beneficiaries enrolled in GCM during a given month, this can however take up to 40 to 60 minutes per month and the full scope of services must be met. Services must be delivered during that billing month and cannot be applied to future program months.
Is a Certified Medical Assistant qualified to do the assessment or re-assessment required by CMS to bill for this CPT code?
No, only RNs can provide these services to your patients if not completed by a physician or mid-level. If you read and understand the full scope of services needed to provide CCM services to patients on a monthly basis an MA or an LPN does not qualify to fully provide these services. They cannot assess or reassess the patient in order to offer the appropriate guidance and support to the CCM patients. By selecting MAs or LPNs you are ultimately placing more work back on the practice and not being compliant under law for using the proper licensed clinical staff to put together the comprehensive care plan required in order to begin billing for CCM services. Additionally, you can be placing your patients at risk. CMS refers you to the CPT definition of “clinical staff”. Clinical staff is defined as a person who, under the supervision of a practitioner, is allowed by law, regulation, or facility policy to perform or assist in the performance of a specified action and holds licensure in the state where providing services.
It is important if you decide to work with a care management services firm to understand the staff they will be using to perform CCM services. Some firms are using CNAs, MAs and LPNs to provide the care planning services. If you are to be audited you would fail if the audit trail was reviewed since these individuals are not legally allowed to provide care planning services, access or reaccess a patient which is part of the scope of services for CCM.
Does non face-to-face care need to be delivered "outside of the office"?
Non-face-to-face care management services may be furnished inside or outside of the provider’s office. Clinical staff must perform these services under the general supervision of a physician. Which is why providers and healthcare organizations can work with care management services firms like our to provide these comprehensive services to their patients as an extension of their practice.
What is the reimbursement for the G0511 CPT Code for RHCs and FQHCs?
The 2021 rate for GCM services in RHCs and FQHCs is $79.26. The rate is available using the PFS Lookup tool here.
Is the coinsurance/deductible waived for GCM services billed by a RHC or FQHC?
No. The coinsurance/deductible applies to GCM services.
Can Rural Health Centers (RHCs) and Federally Qualified Health Centers (FQHCs) work with a Care Management Services Vendor to provide these services to their patients?
Rural Health Centers (RHCs) and Federally Qualified Health Centers (FQHCs) can work with a Care Management Services Vendor to provide these services to their patients under general supervision.